
Every day, 17.6 veterans die by suicide. This heartbreaking number from the latest VA report highlights a crisis, but it points to a deeper systemic issue: the Rating Gap.
While one in three veterans carries a diagnosed mental health disorder, thousands receive low Department of Veterans Affairs disability ratings or outright denials. They have the diagnosis but lack the strategy to prove service connection.
From our experience, this gap leaves too many veterans struggling to adapt to civilian life without crucial support. Understanding the current veterans mental health statistics is the first step to change.
This piece fits into our bigger look at veterans statistics. Check out our last article on what percentage of the homeless population are veterans. Our next one dives into what percentage of veterans are female.
Here, we equip you to stay informed and bridge that gap. This article gives many veterans the knowledge to secure the rating and care they earned.
Key Points
- Veteran suicide rates remain higher than the general population, especially among veterans not enrolled in VA care.
- Early mental health treatment and consistent follow-up lower risk and improve long-term outcomes.
- Recent VA rating changes make documentation and functional impact more important than diagnosis alone.
- Many claims fail due to missing service connection evidence, not lack of eligibility.
- Clear guidance and timely support help veterans avoid being underrated or overlooked.
Current Veterans Mental Health Statistics: The 2025 Data Brief
Numbers cut through noise. This section lays out the cold, hard facts behind today’s veterans’ mental health statistics, using the most recent federal data to show where risks concentrate and why context matters.
The Big Picture on Mental Health Status
Federal reporting continues to show that suicide rates among veterans remain higher than non veterans, even after modest declines in recent years.
Male veterans account for the majority of deaths, while female veterans face a faster-growing rate increase. Age, access to care, and social isolation remain top risk factors.
From our work reviewing claims data, patterns repeat. Veterans who served during Operation Enduring Freedom and the post-9/11 era, including Iraq and Afghanistan veterans, report higher rates of anxiety and trauma-related symptoms.
Older veterans from the Vietnam War era still represent the largest number of total deaths due to population size, even though younger cohorts show higher proportional risk.
Survivors from World War II remain statistically small today, yet their long-term mental health outcomes shaped modern VA policy.
Veterans vs. the General Population
According to the National Institute of Mental Health and the Substance Abuse and Mental Health Services Administration, veterans consistently report worse mental health status than civilians. Exposure history, repeated deployments, and barriers to care explain much of the gap.
Prevalence Comparison (Latest Aggregated Data)
| Condition | Veterans | General Population |
| Posttraumatic stress disorder | ~11–15% | ~6% |
| Major depression | ~14% | ~8% |
| Anxiety disorders | ~19% | ~15% |
For instance, a former infantryman from Afghanistan may report sleep disruption and irritability years after discharge, while a Vietnam-era veteran might face chronic depression tied to delayed treatment. Different eras, similar outcomes.
What These Numbers Mean
Data from the mental health services administration confirm one takeaway. Diagnosis rates rise when access improves. Treatment outcomes improve when care starts early. Statistics do not tell the full story, but they show where systems strain and where intervention saves lives.
As one public health expert once said, “What gets measured gets managed.” The numbers point clearly to where attention must go next.
The 2026 Shift: How VA Rating Changes Affect Mental Health Claims
Policy updates in 2026 mark a real shift in how veterans affairs evaluates mental health conditions. Understanding this change helps veterans protect ratings and access the mental health support they need.
The Five Functional Domains Explained
The VA now evaluates mental health through five functional domains:
- Cognition and memory
- Interpersonal relationships
- Task persistence and pace
- Adaptation and stress tolerance
- Self-management
This framework focuses less on labels and more on daily impact. PTSD symptoms, for example, matter most when tied to work limits, strained family ties, or safety concerns.
No More 0% Ratings
One major update stands out. The VA is eliminating the 0% mental health rating. Any service-connected condition should qualify for at least a 10% rating. Higher ratings such as 70% rating or 100% rating depend on functional impairment, not diagnosis alone.
We see this play out often. A veteran discharged from active duty with documented anxiety may now receive compensation where none existed before. That’s progress, but it raises the bar for evidence.
Why Documentation Matters More Than Ever
These changes increase the importance of clear records showing mental health needs over time. For example, therapy notes describing missed workdays carry more weight than a single exam. Statements from spouses or coworkers often help explain real-world limits.
Consider this question: How does the condition affect mornings, focus, or stress response? The VA now asks that too.
As one former VA clinician put it, “Function tells the story.” Veterans who understand that story stand a better chance of receiving fair outcomes and consistent mental health support.

Veteran Suicide Statistics: A Look at the Current Landscape
We dive into the raw veteran suicide statistics here. Think of this as your quick guide to the numbers shaping suicide rates today. We’ll cover totals, gender splits, and why enrollment in VA care matters so much.
The Total Toll in 2022
Back in 2022, the latest full year with verified data, 6,407 veterans lost their lives to suicide. That shakes us every time we review it. These figures come straight from the Department of Veterans Affairs annual report.
They show a stubborn challenge in mental health status for those who’ve served.
Gender Breakdowns That Demand Attention
Male veterans faced a rate of 37.3 per 100,000 in 2022. Female veterans saw 13.5 per 100,000. Compare that to non-veterans. Men outside service hit 28.7, women just 7.2. Folks, the gap screams for action.
As the National Institute of Mental Health notes, these disparities tie back to unique service stresses.
Ever ask yourself why healthcare providers push early check-ins? Simple. Veterans not linked to VA systems show rates up to twice as high. We see it in claims all the time.
Why Enrollment Changes the Game
Picture a vet skipping VA enrollment due to stigma. Their risk spikes. The National Center for PTSD backs this. Enrolled vets get tools like therapy that cut odds.
For example, one client we helped enrolled after a close call. His mental health status turned around with consistent support. Grab that lifeline. It saves lives.
The “22 a Day” Metric: Fact vs. Fiction in 2026
That “22 a day” line? It sticks in your head like a bad earworm from boot camp. We get why the veteran suicide community rallies around it. Born from a 2012 Department of Veterans Affairs study on military members, it captured the heartbreak.
The Real Count Today
Fast forward to now. The true average sits at 17.6 commit suicide cases daily. That’s from the 6,407 total in 2022. Sure, a dip from the old peak. Yet don’t pop the champagne yet. Risk factors like solo living in remote spots or skyrocketing bills keep the fire hot.
Keeping the Urgency Front and Center
We respect the “22” for sparking talks. As vet advocate Jon Stewart once quipped, “The enemy is noise; the goal is clarity.” Spot on.
Isolation hits hard post-service. Cost of living? It’s squeezing people tight. For instance, a buddy shared how rent hikes pushed him toward dark thoughts until he dialed the crisis line.
What if we flipped the script? Track those risk factors early. Chat with a peer. Small moves build big shields. The drop proves prevention works. Let’s push for more!
Veteran Suicide Rate by Year: Analyzing the Trends
Tracking veteran suicide rate by year feels like charting a storm’s path. We pull from fiscal year data to spot rises, dips, and what they mean for eras like post-9/11. This sets up our line graph below for a clear visual punch.
The Climb and Hold Steady
From 2001’s 23.3 per 100,000, suicide rates climbed steady through 2018 at 33.3. Then a plateau kicked in. Fiscal year 2024 reports show 34.7 for 2022, barely budging. Why the stall? Better outreach, maybe. But we know access lags in rural zones.
- 2001: 23.3 rate
- 2010: 28.8
- 2018: 33.3 peak
- 2022: 34.7
These numbers ground us. They remind teams like ours to tweak claims advice for mental health ties.

Era Spotlights: Who Bears the Brunt
Iraq and Afghanistan veterans lead in rates, especially those aged 18–34. For these younger guys, the rate clocks in at 47.6 per 100,000—the highest of any age group.
Total deaths? Those tilt toward Vietnam War veterans and those over 55. In fact, veterans aged 55+ accounted for nearly 60% of all suicides in 2022, totaling 3,860 losses.
Even our oldest heroes, the World War II survivors in the 75+ bracket saw a sharp 4.9% increase in their suicide rate.
Hypothetical: You’re a Gulf War vet eyeing trends. Does your era’s data nudge you to file that claim? It should. For example, we guided a Vietnam-era client through secondary PTSD links. His rating jumped, easing daily strains.
As General Colin Powell said, “The day the soldiers stop bringing you their problems is the day you stop leading them.” Leaders, that’s us all. Use these trends. Connect dots in service records. One solid stressor note can unlock care.
Here’s a quick line graph of those rates. See the steady creep, then flatline? That’s our call to action.
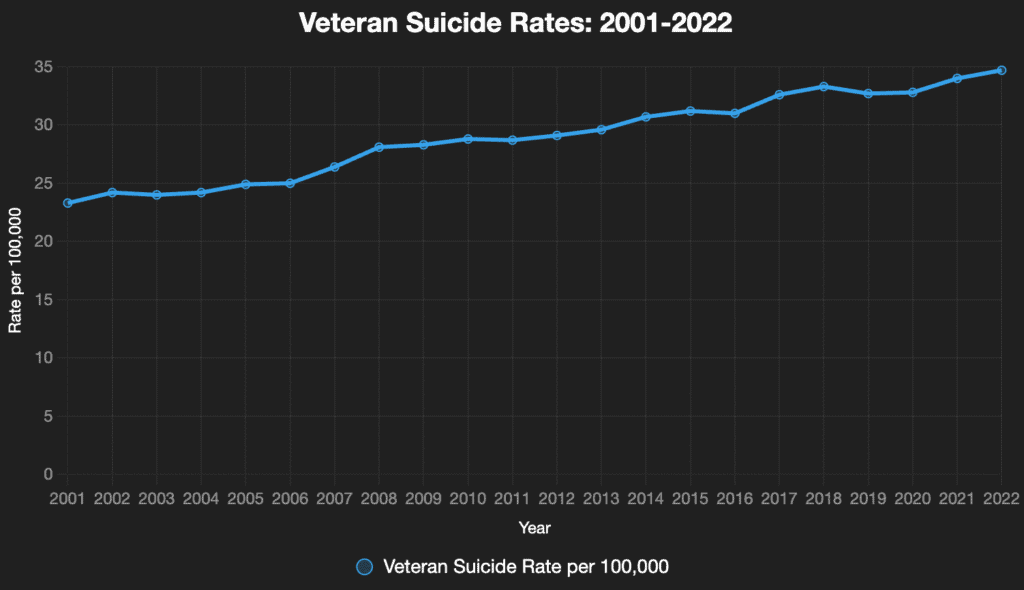
Source for the statistics: U.S. Department of Veterans Affairs, Office of Mental Health and Suicide Prevention. (2024). 2024 National Veteran Suicide Prevention Annual Report.
Veteran Suicide Rates: Risk Factors and Prevention
We shift gears from those stark numbers to real steps forward. This section spotlights key risk factors behind veteran suicide rates. We’ll unpack triggers like combat exposure and explore suicide prevention tools, including vital mental health services.
Triggers That Linger Long After Service
Combat exposure plants seeds for trouble. Think blasts, buddy losses, endless patrols. These hit military service members deep. They spark suicidal thoughts that creep in during quiet nights.
Data shows vets with heavy exposure face 4 times higher odds. One study pegged it at 20% carrying chronic PTSD from Iraq tours alone.
Ever wonder why some shake it off quicker? Support timing matters. Delay it, and thoughts darken fast.
Building Shields Through Targeted Support
Mental health support flips the script. Start with peer groups; research shows they drastically cut isolation by providing a sense of shared military service. We often nudge clients toward tools like the PTSD Coach app for daily check-ins. This builds healthy habits before a crisis can brew.
If you find yourself in a dark place, dial the Veterans Crisis Line at 988, then press 1. It’s 24/7, confidential, and connects you to trained responders who understand the unique needs of military service members.
Beyond clinical care, strategy matters. As Senator Tammy Duckworth put it, “Veterans shouldn’t fight a second battle for care they earned.” Bureaucracy and long waits for mental health services can leave folks hanging.
This is why we push for pre-filing nexus letters and documented service journals. These tools speed up the veterans affairs approval process, ensuring you don’t have to wait for the support you’ve already paid for in service.
Beyond the Numbers: Turning Stats into a Successful VA Claim
Stats sting, sure. But they fuel action, too. Here we connect dots from diagnosis to dollars, tips on the fresh 2025/2026 VA Rating Changes, plus ways to tie posttraumatic stress disorder and major depression to roots like military sexual trauma.
The Five Functional Domains: A Fairer Yardstick
The VA has moved past the fuzzy “social impairment” criteria for the Five Functional Domains of the past. The new model scores you on Cognition, Interpersonal Interactions, Task Completion, Navigating Environments, and Self-Care.
Each gets a score from 0–4. This shift captures the “daily slips” that the old system missed, such as a veteran who can hold a job but struggles with basic self-care or navigating public spaces.
No More Zeroes: The 10% Floor Explained
Big win: VA has axed the 0% mental health rating. Now, every service-connected mental health disorder nets at least 10% compensation. If you were previously rated at 0%, now is the time to act.
While your current rating is “grandfathered,” filing a supplemental claim under the 2026 rules could trigger an immediate increase to the new minimum—or higher.
Secondary Links That Boost Your Case
PTSD symptoms often tag along with traumatic brain injury (TBI) because blasts frequently cause both.
While the VA prevents “pyramiding” (rating the same symptom twice), you can often claim TBI as primary and PTSD as secondary if your doctors can distinguish between cognitive “fog” and emotional “trauma.”

Data from the National Center shows that major depression follows military sexual trauma (MST) in a significant number of cases. In fact, nearly 40% of veterans who disclose MST to the VA are men, and depression is the most common co-diagnosis.
A strong nexus letter—a medical link from your provider—is the seal that proves these conditions are “at least as likely as not” related to your service.
Pro-Tip: Use VERA for Free Reviews. Don’t just guess if your claim is ready. Use the Visitor Engagement Reporting Application (VERA) to schedule a call with a Regional Office rep. They can often spot gaps in your medical evidence before you hit “submit.”
Strategic Claim Tips (Updated for 2026)
The “Five Functional Domains” model mentioned earlier is your best friend here. When preparing for a C&P exam, don’t just list symptoms—map them to these buckets:
- Mapping to Domains: Instead of saying “I’m sad,” say “My depression causes Moderate Impairment in the Interpersonal Domain; I avoid my family 25% of the time.”
- Mirroring Language: Use terms found in the VASRD (38 CFR Part 4). Use words like “clinically significant,” “interference with task completion,” and “frequency of impairment.”
- Tracking with Apps: Use Daylio or the PTSD Coach app to export a 30-day “Mood Map.” Presenting a printed log of your daily “slips” to an examiner is much more powerful than trying to remember your worst day on the spot.
As Maya Angelou noted, “You may not control all the events that happen to you, but you can decide not to be reduced by them.”
Final Thoughts
Those veterans mental health statistics we covered? They stand for actual people. Every number hides a story that could end differently with the right push. We see more veterans stepping up these days.
They ditch the mental health stigma that whispers “tough it out.” Instead, they grab the treatment and back pay they deserve. Picture this: You skip that old shame. You chat with loved ones about the rough spots, and relief follows quickly.
Supporting veteran mental health starts small. Check online resources like VA chat lines. Book a session and file that claim. One move snowballs into stability.
Hey, veterans, why wait? Head to our homepage now for your free evaluation. Unlock what you earned. Real help remains available, and it starts with one smart step forward.



